My Specialty
Respiratory Telemetry Nursing, Doug Robinson, USC Arcadia Hospital
Leading a close-knit unit through the COVID-19 crisis and beyond
Doug Robinson, RN, MSN
Nursing Manager
4-North Respiratory Telemetry Unit
USC Arcadia Hospital
Please share with us the arc of your nursing career.
My journey began in the Seattle area. After I had some experience under my belt, I accepted a travel nursing assignment in the ICU, which brought me to Southern California.
After years of working in ICU, I ventured into medical sales, specific to the wound care market. I never really felt like I was selling because I had used the products in my own practice and was able to draw on my nursing experience and my experience with patient education. This part of the journey also allowed me to travel all over the country, including to Puerto Rico.
Eventually, I decided I wanted to pursue a graduate degree in nursing. Originally, I meant to focus my master’s degree on education, but because I found myself in many leadership roles throughout my career and found satisfaction in that work, I changed my focus to leadership.
Tell us about your unit.
The 4-North (4N) respiratory telemetry unit is a busy 40-bed unit that focuses on patients presenting with a primary respiratory issue. Many respiratory patients have multi-organ system failures and multiple comorbidities, like renal failure needing dialysis. It’s common for them to be on ventilators and have tracheostomies or gastric tubes. Thus, these patients tend to be high-acuity and need assistance with their activities of daily life.
What brought you to this particular unit and nursing specialty?
I was very familiar with the care of patients on ventilators, so this unit was a natural fit. And, honestly, throughout my career, I’ve always been at the right place at the right time.
How did the COVID-19 pandemic impact your unit?
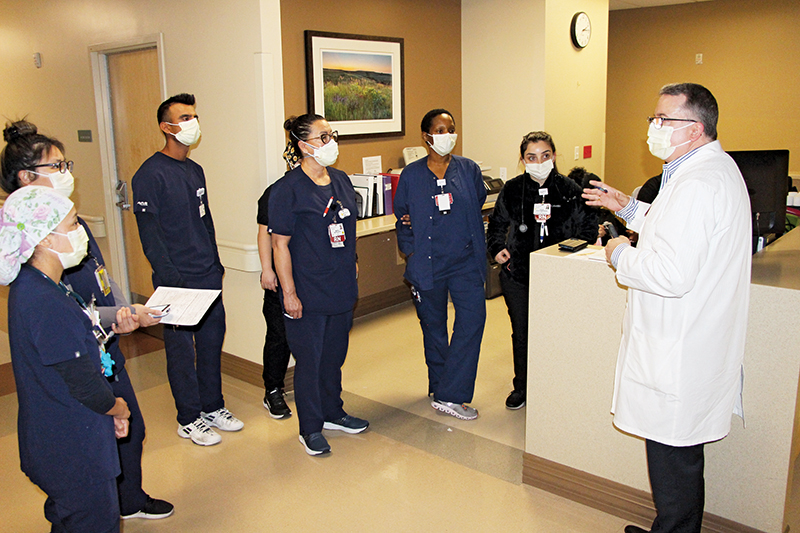
My unit, 4N, was basically the epicenter for treating the COVID-19 medical-surgical population at USC Arcadia Hospital. It was a very challenging time for the staff. As the leader of this unit, I was committed to being visible and present with my staff and patients. Conducting daily huddles for both shifts helped all employees know they were supported.