My Specialty
Intensive Care Unit, Ana Campos, Redlands Community Hospital
Caring for critically ill patients from birth through end of life
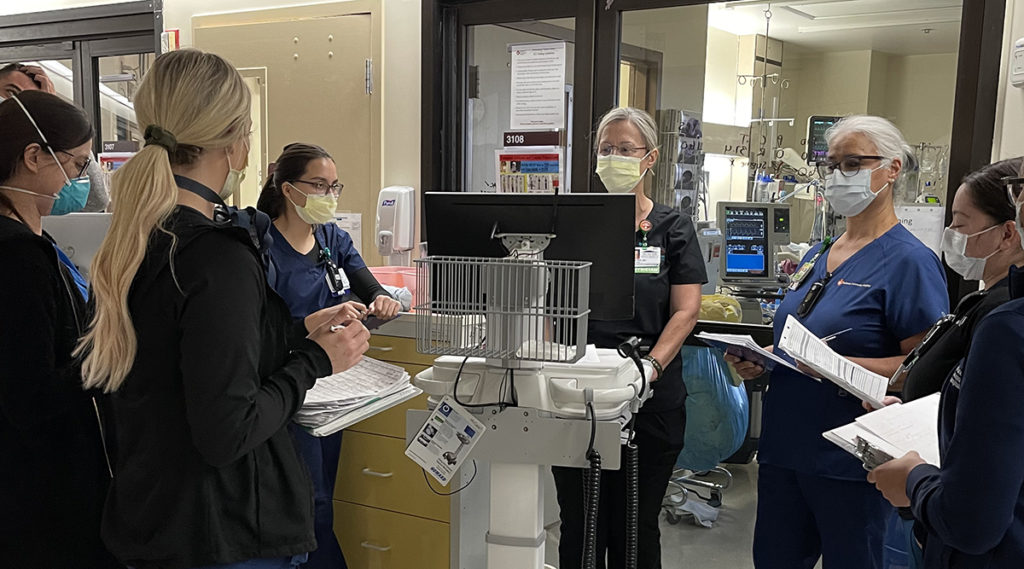
Ana Campos, RN, BSN, CCRN
ICU Manager
Redlands Community Hospital
Please share the arc of your nursing career with us.
I have been a nurse for 45 years. I studied nursing in Peru and worked there for 10 years in academia as a clinical instructor. I also served as a clinician in telemetry and cardiothoracic positions. I moved to the United States around 35 years ago, applied for a position in the intensive care unit at Redlands and have happily been here ever since.
What has your career been like at Redlands?
I started as a staff nurse on nights and then moved to day shift. I frequently took on the role of charge nurse while still carrying a patient load. At a certain point, I naturally slid right into the position of ICU unit manager. No one prepares you to be a nurse manager — I tried it and liked it, and I continue to enjoy my position to this day. (Nurse managers at Redlands are now sent to the classes with the ACNL Foundation for Nurse Leaders.)
How was nursing different between the U.S. and Peru?
The nursing education process was quite similar. In Peru, we did not have access to the technology and monitoring systems that were common in the U.S., so encountering those when I arrived was definitely the major difference. However, the ways in which we provide patient care are essentially the same.
What cultural differences have you found?
I was so fortunate to come to this hospital, where I felt welcome from the very first day. My colleagues truly took the time to listen and understand me. If we ran into situations where they couldn’t understand my accent, they patiently helped me find other ways to make myself understood.
Redlands continues to be a very diverse community hospital. I have had the pleasure of working with nurses from India and many other countries; the Filipino community is very strong here. Our diversity is helpful in meeting the needs of our patients and their families and in providing culturally relevant approaches to health and wellness.
What advice would you have for nurses coming to the U.S. from other countries?
I would definitely say that you need to study and learn everything you can. After every shift, I would always reflect and write a summary of my day, taking note of what I needed to review and brush up on. You need to get accustomed to the uses of technology here in the U.S., know where everything is, understand how things work and engage in nonstop learning.