My Specialty
Psychiatric Emergency Nursing, Sandy Kesler-Newman, Arrowhead Regional Medical Center
Caring for vulnerable behavioral health patients
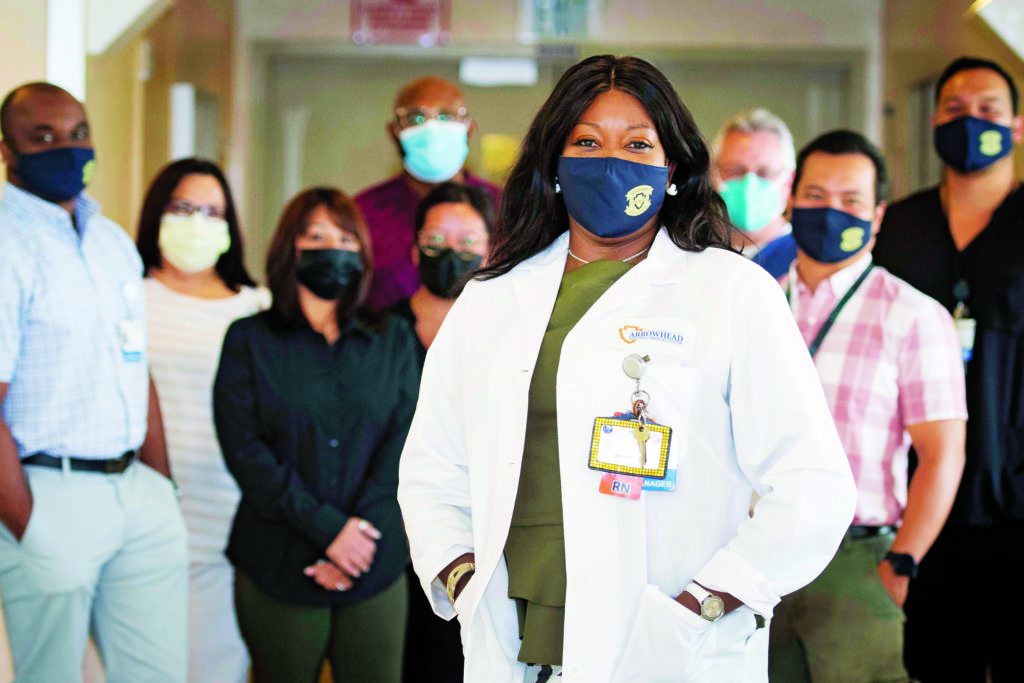
Sandy Kesler-Newman, RN, BSN, PHN
Unit Manager, Psychiatric Emergency Department
Arrowhead Regional Medical Center, Colton
Tell us about the trajectory of your life and career.
I have been a nurse 33 years, 22 of which were in the ED. The way I got my job at Arrowhead Regional Medical Center is a funny story: I was in a car accident and went to the ARMC emergency department to be treated. I started talking with a nurse manager who inquired about my work experience. Soon after, I was hired to work here in the ED!
After a couple of years as a charge nurse and then assistant nurse manager in the ED, I was asked to coordinate the new Medical Indigent Program, which was established using funds the Obama administration had made available for low-income healthcare. I love building new programs, so this was a great challenge.
From there, I became a nurse educator for heart failure patients. Then, in 2019, I received a phone call saying the Behavioral Health Department needed help building its medical aspect. I had no behavioral health experience, but I thought I could be a good liaison between the medical and psychiatric sides of the ED.
Here I am two years later, and I love it. I’m still considered the liaison, but I’m also the unit manager for the psychiatric ED.
What are your main responsibilities?
I make sure my department runs efficiently and safely on all levels. I have several assistant managers who report to me, along with two charge nurses; I call them my executive team. One of my responsibilities is building our staff’s capacity so that patients’ behavioral and medical issues are equally addressed.
Behavioral health issues can be triggered by underlying medical issues — blood sugar or thyroid problems, for example — so providing highly therapeutic care for these vulnerable patients means assessing and treating them holistically.
What populations do you serve?
We serve San Bernardino County and beyond. The homeless population in our county is very high, but there’s a great deal of chronic mental illness among people from all walks of life, as well as untreated underlying comorbidities and significant psychiatric disabilities.
We build trust on a daily basis with a patient population aged 18–64. Many of our patients are “frequent flyers” we know by name. When they return for another visit, we start building trust all over again. I say to them, “Remember me? I’m Sandy. We’re here for you.”



